Metabolic Syndrome: The Silent Precursor Epidemic and How to Reverse It
Metabolic Syndrome: The Silent Precursor Epidemic and How to Reverse It
Imagine your body as a sophisticated control center. Suddenly, five different alarm panels start flashing: high blood pressure, elevated blood sugar, excess abdominal fat, high triglycerides, and low HDL cholesterol. Individually, each is a concern. Together, they represent a full-scale emergency—a coordinated system failure known as metabolic syndrome
This isn't a rare disorder; it's a silent precursor epidemic. According to the American Heart Association, approximately one in three American adults meets the criteria. Yet, most are unaware they have it, walking unknowingly toward a cliff of type 2 diabetes, heart attack, and stroke. The powerful truth, however, is that this syndrome is primarily a lifestyle-coded condition. Through the precise lens of therapeutic nutrition and public health science, we can learn not just to manage these alarms, but to silence them at their source. This article moves beyond symptom lists to explore the unifying mechanism of metabolic dysfunction and provide a actionable blueprint for systemic reversal
Decoding the Syndrome – More Than the Sum of Its Parts
Metabolic syndrome is diagnosed when an individual presents with at least three of the five key risk factors, as defined by the National Cholesterol Education Program (NCEP ATP III)
Abdominal Obesity: Waist circumference >40 inches (men) or >35 inches (women)
Elevated Triglycerides: ≥150 mg/dL
Reduced HDL Cholesterol: <40 mg/dL (men) or <50 mg/dL (women)
Elevated Blood Pressure: ≥130/85 mmHg
Elevated Fasting Glucose: ≥100 mg/dL
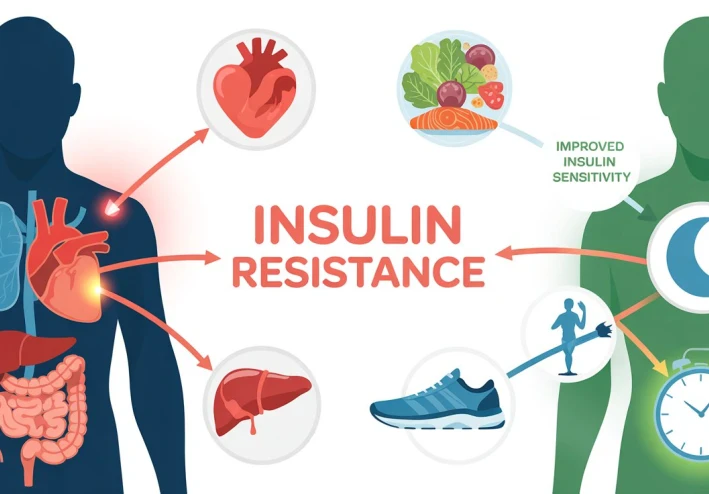
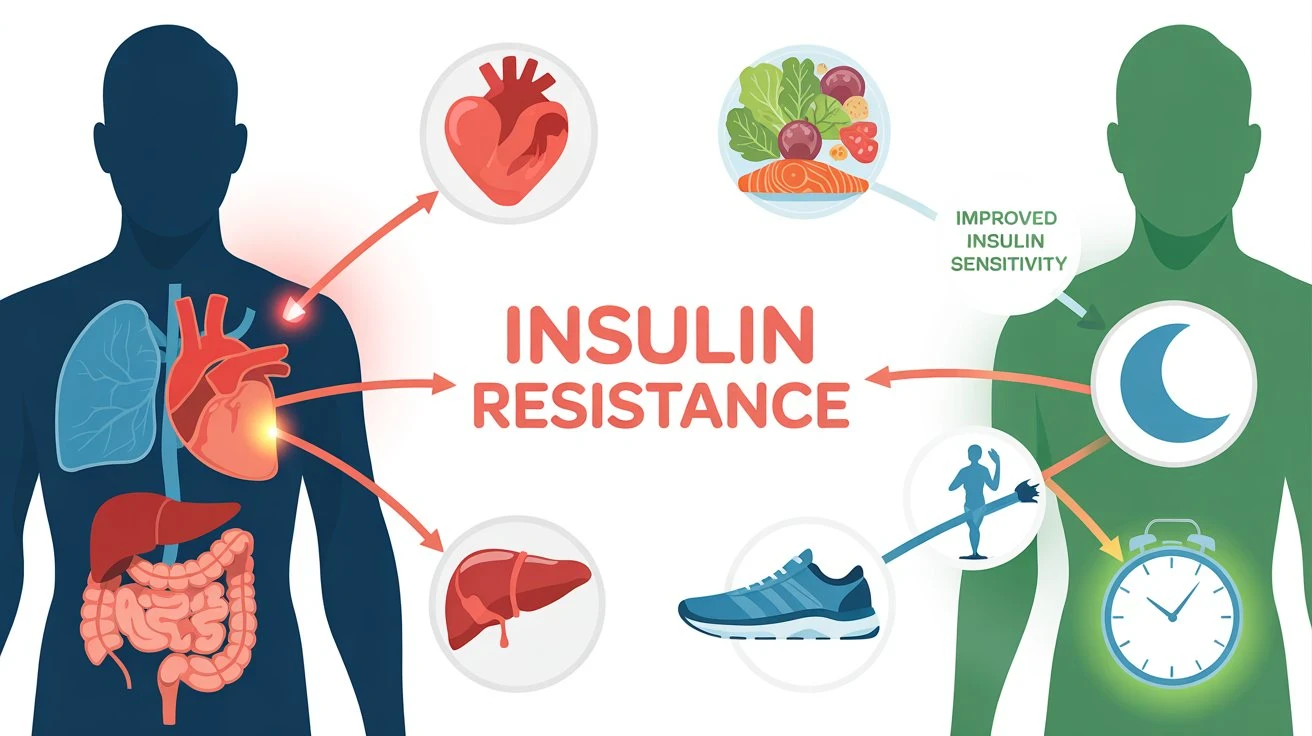
The critical insight is that these are not separate issues. They are interconnected symptoms of a core problem: insulin resistance. When your cells become deaf to the hormone insulin, which ushers glucose out of the bloodstream, your pancreas pumps out more, creating a cascade of metabolic havoc: fat gets stored centrally, triglycerides rise, blood pressure increases, and inflammation becomes chronic. This is the unifying pathophysiology that turns separate metrics into a syndrome
The Core Mechanism – Insulin Resistance as the Conductor
Think of insulin as a master key designed to unlock your cells to receive energy (glucose). In insulin resistance, the locks become rusty. The body's response? Produce even more master keys (insulin). This hyperinsulinemia is the root driver
Fat Storage Directive: High insulin signals your body to store fat, preferentially in the visceral area around your organs—the most dangerous type of fat, which itself pumps out inflammatory cytokines
Lipid Dysregulation: It stimulates the liver to produce more triglycerides while inhibiting the clearance of blood fats
Blood Pressure Impact: It promotes sodium retention in the kidneys and stimulates the sympathetic nervous system, raising blood pressure
Inflammatory State: The resulting visceral fat and high blood sugar create a pro-inflammatory, pro-oxidative environment that damages blood vessels
Therefore, the primary goal of any intervention is to improve insulin sensitivity. This is where food shifts from mere fuel to targeted therapeutic agent
Food as a Signal, Not Just Calories
Modern nutrition science has moved beyond "calories in, calories out." We now understand that food sends hormonal and genetic instructions to our body. For metabolic syndrome, we must send the right memos
The Fiber Imperative: Soluble fiber (from oats, legumes, apples, flaxseed) is a cornerstone. It forms a gel in the gut, slowing sugar absorption and blunting the post-meal insulin spike. A study in the Journal of Nutrition consistently shows that increased soluble fiber intake is directly linked to improved insulin sensitivity and lower visceral fat
The Right Fats: Replacing inflammatory fats (processed seed oils, trans fats) with anti-inflammatory monounsaturated and omega-3 fats (olive oil, avocados, fatty fish) directly improves lipid profiles and reduces the inflammation that worsens insulin resistance. The landmark PREDIMED trial demonstrated that a Mediterranean diet rich in olive oil and nuts dramatically reduced the incidence of major cardiovascular events in at-risk individuals
Carbohydrate Quality & Timing: The goal is not necessarily ultra-low-carb, but smart-carb. Emphasizing low-glycemic, whole-food sources (berries, leafy greens, quinoa) and being mindful of timing (e.g., consuming most carbs around physical activity) can help manage glucose load. The glycemic load of a meal is a more practical metric than the glycemic index alone
The Therapeutic Nutrition Protocol – A Four-Pillar Approach
Reversing metabolic syndrome requires a systemic reset built on these pillars
The Plate Pattern: Adopt a modified Mediterranean or Portfolio Diet framework. Visualize your plate: 50% non-starchy vegetables, 25% quality protein (legumes, fish, poultry), 25% high-fiber whole grains or starchy vegetables, with a drizzle of healthy fat
Nutrient Synergy Champions: Focus on specific functional foods
Berries & Cherries: Rich in anthocyanins that improve glucose metabolism
Cinnamon & Turmeric: Shown in meta-analyses to modestly lower fasting glucose and combat inflammation
Vinegar: Acetic acid (1-2 tbsp before a meal) can improve insulin sensitivity by 20-30% for the following meal, per several small human studies
Green Tea: EGCG can enhance fat oxidation and metabolic rate
The Non-Negotiables: Sleep & Movement
Sleep Hygiene: Chronic sleep deprivation (<7 hours) directly causes insulin resistance and increases hunger hormones. Prioritizing sleep is non-negotiable metabolic medicine
Movement Snacking: While regular aerobic exercise is key, recent research highlights the power of breaking up prolonged sitting every 30 minutes with 2-3 minutes of light movement to improve glucose clearance
The Circadian Rhythm Factor: Align eating with your natural clock. Practice time-restricted eating (e.g., a 10-12 hour eating window) to give your insulin system a prolonged daily rest, which has been shown to reduce visceral fat and improve insulin sensitivity independent of calories
From Syndrome to Symphony
Metabolic syndrome is the body's desperate flare gun, signaling that its systems are overwhelmed. But this diagnosis, far from a life sentence, is perhaps one of modern medicine's most actionable redirections. It reveals the levers we can pull. By shifting our perspective from caloric reduction to metabolic resynchronization, we empower ourselves
We move from being passive patients managing separate numbers to active architects of our internal environment. Through the strategic, evidence-based application of therapeutic nutrition—prioritizing food as a precise signal, respecting circadian biology, and integrating purposeful movement—we can quiet the alarms. The goal is not just to avoid disease, but to cultivate a state of metabolic flexibility, where the body efficiently and gracefully switches between fuel sources, energy is sustained, and inflammation is minimized. This is the true reversal: turning a syndrome of discord into a symphony of resilient health
Frequently Asked Questions (FAQs)
Q1: Can you reverse metabolic syndrome completely
A1: Yes, in many cases, metabolic syndrome is entirely reversible through consistent lifestyle intervention. Studies show that losing 5-10% of body weight, increasing physical activity, and adopting a whole-foods, fiber-rich diet can normalize blood pressure, blood sugar, and lipids, effectively dissolving the diagnosis
Q2: Is metabolic syndrome the same as pre-diabetes
A2: They are closely related but not identical. Pre-diabetes specifically refers to elevated blood sugar. Metabolic syndrome includes pre-diabetes as one of its five possible components but requires at least two additional risk factors. Think of metabolic syndrome as a broader state of systemic metabolic dysfunction, with pre-diabetes often being a key feature
Q3: Do I need to go on a very low-carb or ketogenic diet
A3: Not necessarily. While low-carb diets can be effective for rapid glucose control, the long-term data for cardiovascular health is mixed. A sustainable approach for most is a moderate-carb, high-quality-carb diet focused on fiber, healthy fats, and protein. The key is eliminating refined sugars and processed grains
Q4: Are there specific tests I should ask my doctor for beyond the standard ones
A4: Yes. Request a fasting insulin test. While fasting glucose diagnoses pre-diabetes, fasting insulin can reveal insulin resistance years earlier. A high insulin level with normal glucose is a critical early warning sign. Also, ask for an ApoB test for a more accurate assessment of heart disease risk from lipids
Q5: How long does it take to see improvements
A5: Metabolic improvements can begin quickly. Insulin sensitivity can improve within days of dietary changes. Blood pressure may drop in weeks. Significant changes in triglycerides and HDL cholesterol are typically seen within 2-3 months of consistent lifestyle modification