Your Liver is Not a Storage Unit: Reversing Non-Alcoholic Fatty Liver Disease
Your Liver is Not a Storage Unit: Reversing Non-Alcoholic Fatty Liver Disease
Within your abdomen lies your body's most industrious and multifaceted organ: the liver. It is a chemical refinery, a detox center, a nutrient processor, and a storage facility—all in one. Yet, in our modern world of abundant calories and processed foods, this vital organ is increasingly being forced into a pathological role: that of a fat storage unit. This condition, known as Non-Alcoholic Fatty Liver Disease (NAFLD), affects an estimated 25% of adults globally, making it the most common chronic liver disease in the world
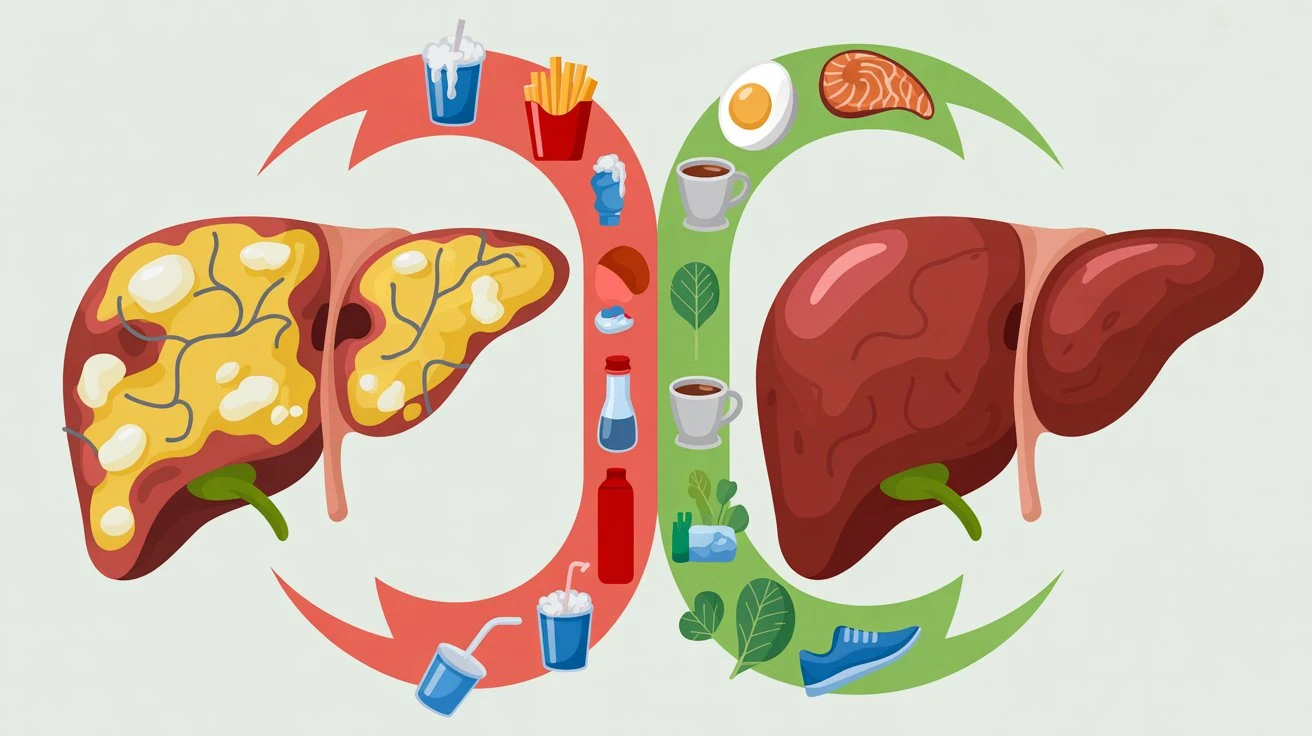
The paradox is profound: a disease of excess rooted in malnutrition—not of calories, but of nutrient quality. NAFLD is not caused by alcohol, but by the standard modern diet and sedentary living. It progresses silently, often with no symptoms until significant damage is done, from simple fat accumulation (steatosis) to inflamed, scarred tissue (NASH and cirrhosis). This article will reframe NAFLD not as an inevitable fate, but as a diet-driven metabolic error that can be corrected. We will explore the precise nutritional levers to pull to shift your liver from a state of passive storage to one of active, healthy metabolism
Understanding NAFLD – More Than Just "Fatty Liver"
NAFLD is defined by the accumulation of excess fat in more than 5% of liver cells, in the absence of significant alcohol consumption. Its more severe form, Non-Alcoholic Steatohepatitis (NASH), involves liver cell damage and inflammation, which can lead to fibrosis, cirrhosis, and liver cancer
The Public Health Scale: The American Liver Foundation notes that NAFLD is a leading cause of liver transplantation. It is intrinsically linked to metabolic syndrome, with insulin resistance being a central driver
The Silent Progression: The liver has no pain receptors. Fatigue and vague right-sided abdominal discomfort may be the only hints, which is why NAFLD is frequently discovered incidentally on routine blood tests showing elevated liver enzymes (ALT, AST)
A Whole-Body Disease: A fatty liver is not an isolated problem. It exacerbates systemic inflammation, worsens insulin resistance, and increases risk for cardiovascular disease. The liver is a central player in metabolic health; when it falters, the entire system is compromised
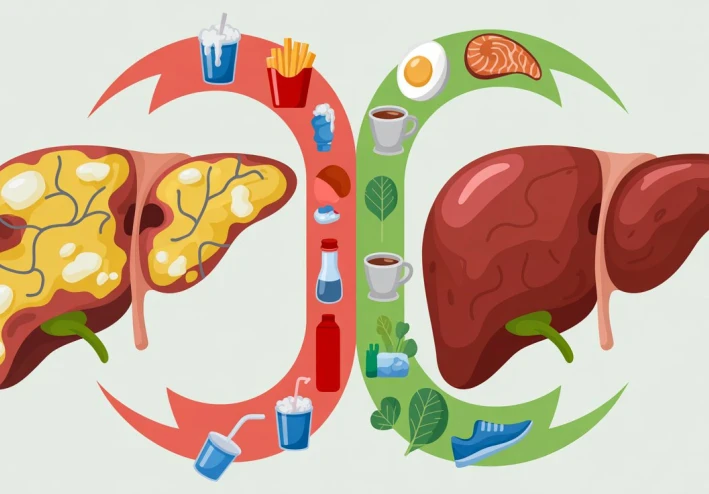
The Nutritional Culprits – How Diet Drives Hepatic Fat
The primary cause of NAFLD is an energy imbalance, but specific dietary components act as potent accelerants
Fructose: The Hepatic Stressor: Unlike glucose, which can be metabolized by all cells, fructose is almost exclusively processed by the liver. In excess—primarily from high-fructose corn syrup in sodas, sweets, and processed foods—it overwhelms the liver's capacity. It is directly converted into liver fat (de novo lipogenesis) and promotes inflammation and oxidative stress. Research in the Journal of Hepatology has consistently linked high fructose intake with NAFLD severity
Refined Carbohydrates & Sugars: White bread, pasta, pastries, and other high-glycemic foods cause rapid spikes in blood glucose and insulin. Chronically high insulin signals the liver to synthesize and store fat
Inflammatory Fats: Diets high in industrial seed oils (soybean, corn, sunflower oil) and processed foods promote an inflammatory state that damages liver cell membranes and fuels the progression from simple steatosis to NASH
The Choline Deficiency Link: Choline is an essential nutrient critical for packaging and exporting fat out of the liver. Modern diets, low in foods like eggs, liver, and soy, are often deficient. Inadequate choline intake can directly cause fat to become trapped in liver cells
Therapeutic Nutrition – The Liver De-Fatting Protocol
The cornerstone of NAFLD reversal is lifestyle medicine, with diet being the most powerful tool. The goal is to reduce the fat-processing burden on the liver and provide the nutrients it needs to heal and export fat
The Foundational Strategy: Weight Loss & Macronutrient Shifts
Modest Weight Loss is Key: A landmark 2015 study in Gastroenterology showed that a 7-10% reduction in body weight can lead to resolution of NASH and regression of fibrosis in a majority of patients. This is the single most effective intervention
Prioritize Quality: Shift from refined carbs to high-fiber, whole-food carbohydrates (vegetables, legumes, low-sugar fruits). Emphasize high-quality proteins (legumes, fish, poultry) and healthy fats (avocado, olive oil, nuts, fatty fish)
Targeted Hepatic Nutrients & Foods (The "Liver-Friendly Pantry")
Choline-Rich Foods: Make eggs, lean beef, chicken, fish, and cruciferous vegetables (broccoli, Brussels sprouts) dietary staples to support fat export
Antioxidant & Anti-Inflammatory Powerhouses
Coffee: Multiple meta-analyses confirm that regular coffee consumption (2-3 cups/day) is associated with a significantly lower risk of NAFLD progression and fibrosis. Chlorogenic acids and other compounds reduce inflammation and fibrosis
Green Tea (EGCG): The catechin EGCG enhances fat oxidation and has direct anti-fibrotic effects in the liver
Turmeric (Curcumin): Potent anti-inflammatory that can lower markers of liver inflammation (ALT, AST)
Berries & Dark Leafy Greens: Provide anthocyanins and other polyphenols that combat oxidative stress in liver cells
Soluble Fiber: Oats, psyllium husk, apples. Fiber binds to bile acids and promotes their excretion, forcing the liver to use cholesterol to make new bile, thereby helping to lower internal fat stores
Fermented Foods: Kimchi, kefir, sauerkraut. A healthy gut microbiome is crucial for the gut-liver axis. Dysbiosis can increase gut permeability, allowing endotoxins to travel to the liver via the portal vein, triggering inflammation. Probiotics can help restore balance
The Crucial Role of Movement
Exercise is independent medicine for the liver. Both aerobic and resistance training have been shown to reduce liver fat content by increasing insulin sensitivity and promoting fatty acid oxidation, even without significant weight loss. Aim for 150+ minutes of moderate activity per week
The Integrated Action Plan – A 4-Phase Approach
Phase 1: Elimination & Assessment (Weeks 1-2): Remove all sources of added sugars, particularly fructose-sweetened beverages and processed snacks. Eliminate refined grains and industrial seed oils. This reduces the immediate fat-production signal
Phase 2: Nourishment & Repletion (Weeks 3-6): Systematically introduce the "Liver-Friendly Pantry" foods. Prioritize choline, fiber, and antioxidants at every meal. Hydrate with water, black coffee, or green tea
Phase 3: Metabolic Retraining (Ongoing): Incorporate regular, daily movement. Practice time-restricted eating (e.g., 12-hour eating window) to give your liver a daily fasting period to process and clear fat
Phase 4: Monitoring & Maintenance: Work with a healthcare provider to track progress via liver enzyme tests (ALT/AST), fibroscan if available, and metabolic markers (fasting insulin, triglycerides). Celebrate non-scale victories like improved energy and clarity
Reclaiming Your Metabolic Command Center
NAFLD is a stark manifestation of a metabolic system pushed past its design limits by the modern food environment. But the liver possesses a remarkable capacity for regeneration and recovery. By understanding the specific dietary drivers—fructose, refined carbs, inflammatory fats, and choline deficiency—we can move from a generalized "healthy diet" to a targeted therapeutic nutrition strategy
This journey is not about deprivation, but about strategic nourishment. It is about choosing foods that actively support the liver's innate functions rather than overwhelming them. By adopting this protocol—centered on whole foods, hepatic nutrients, and consistent movement—you are not just "dieting." You are conducting a systemic renovation of your body's central processing plant, transforming it from a clogged storage depot back into the elegant, efficient metabolic command center it was meant to be. The power to reverse this silent epidemic lies not in a pharmacy, but on your plate
Frequently Asked Questions (FAQs)
Q1: Can NAFLD be completely reversed
A1: Yes, especially in its early stages (simple steatosis). Studies show that with sustained lifestyle changes leading to 7-10% body weight loss, the accumulated liver fat can be mobilized and eliminated, and inflammation can subside, effectively reversing the disease. Even with some fibrosis (scarring), improvement is possible
Q2: How is NAFLD different from alcoholic liver disease
A2: The liver damage looks similar under a microscope, but the cause differs. Alcoholic Liver Disease is caused by excessive alcohol consumption. NAFLD occurs in people who drink little to no alcohol and is primarily driven by metabolic factors: diet, obesity, and insulin resistance
Q3: Are there any specific tests I should ask my doctor for
A3: Beyond standard liver enzymes (ALT, AST)
* FibroScan (VCTE): A non-invasive ultrasound that measures liver stiffness (fibrosis) and fat content
* HbA1c & Fasting Insulin: To assess glucose control and insulin resistance
* Cholesterol Panel: Look for high triglycerides and low HDL
* In some cases, a liver biopsy is the gold standard for diagnosing NASH and staging fibrosis
Q4: Is intermittent fasting helpful for NAFLD
A4: Yes, time-restricted eating (e.g., confining meals to an 8-10 hour window) can be very beneficial. It gives the liver an extended daily period without having to process new nutrients, allowing it to focus on fat metabolism, cellular repair (autophagy), and reducing insulin levels
Q5: What about supplements like milk thistle or vitamin E
A5: Evidence is mixed
* Vitamin E: May be recommended by a hepatologist for non-diabetic adults with biopsy-proven NASH, but high doses have been linked to other risks
* Milk Thistle (Silymarin): Some studies show modest benefits for liver enzymes, but robust evidence for reversing NAFLD is lacking
* General Rule: Always consult your doctor before starting any supplement. The foundation must be dietary and lifestyle change; supplements are not a substitute