Fatty Liver: Causes, Types, Symptoms, Treatment, and the Essential Role of Nutrition
Fatty Liver: Causes, Types, Symptoms, Treatment, and the Essential Role of Nutrition
Introduction: Why Are So Many People Struggling With Fatty Liver Today?
Have you ever wondered why doctors are talking more and more about fatty liver disease in recent years? Just two decades ago, many people rarely heard the term. Today, it seems like everyone knows someone who has it—or maybe even has been diagnosed themselves. This raises important questions: What exactly is fatty liver? Why is it on the rise? Is it just a symptom of another health condition, or is it a disease in its own right? And most importantly, what can be done to manage it—especially through treatment and nutrition?
In this in-depth guide, we will explore every aspect of fatty liver disease, from its causes and types to treatment options and the role of diet. By the end, you’ll understand not just what fatty liver is, but also how to take proactive steps toward reversing it and protecting your liver health for the future.
---
What Is Fatty Liver? Symptom or Disease?
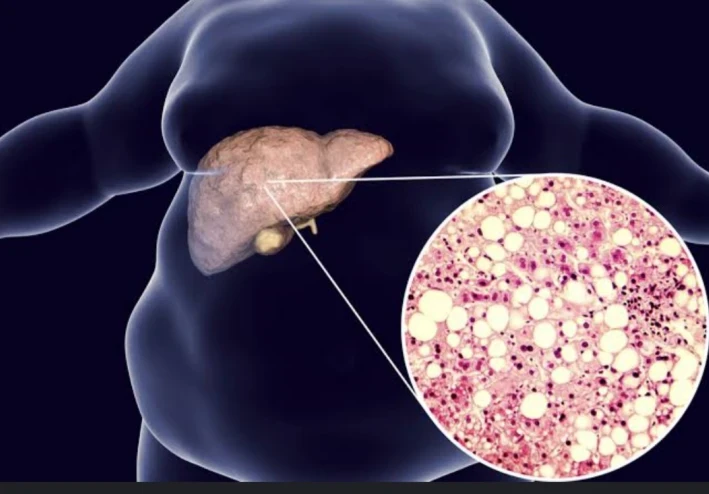
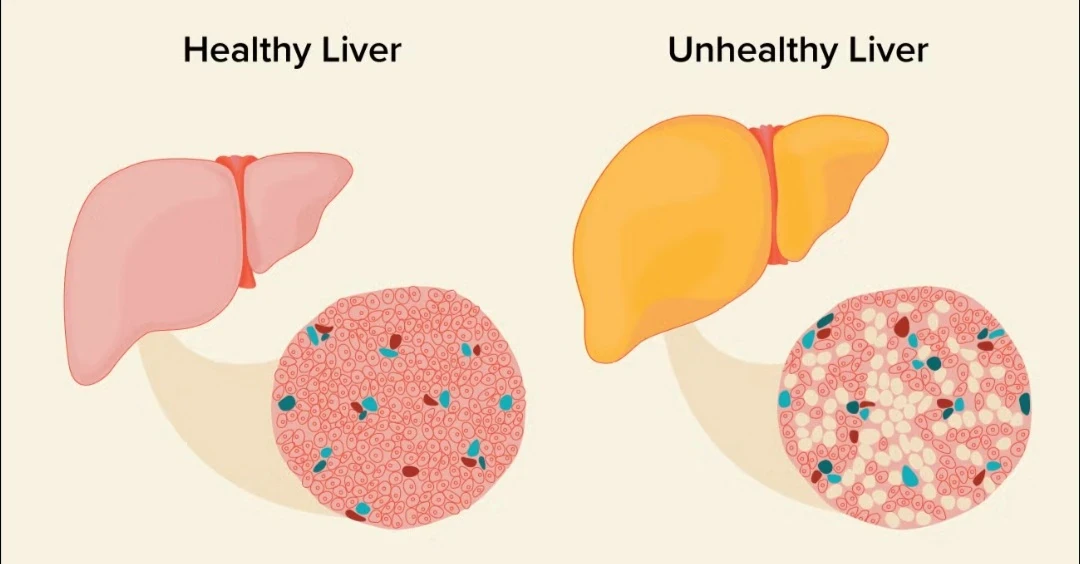
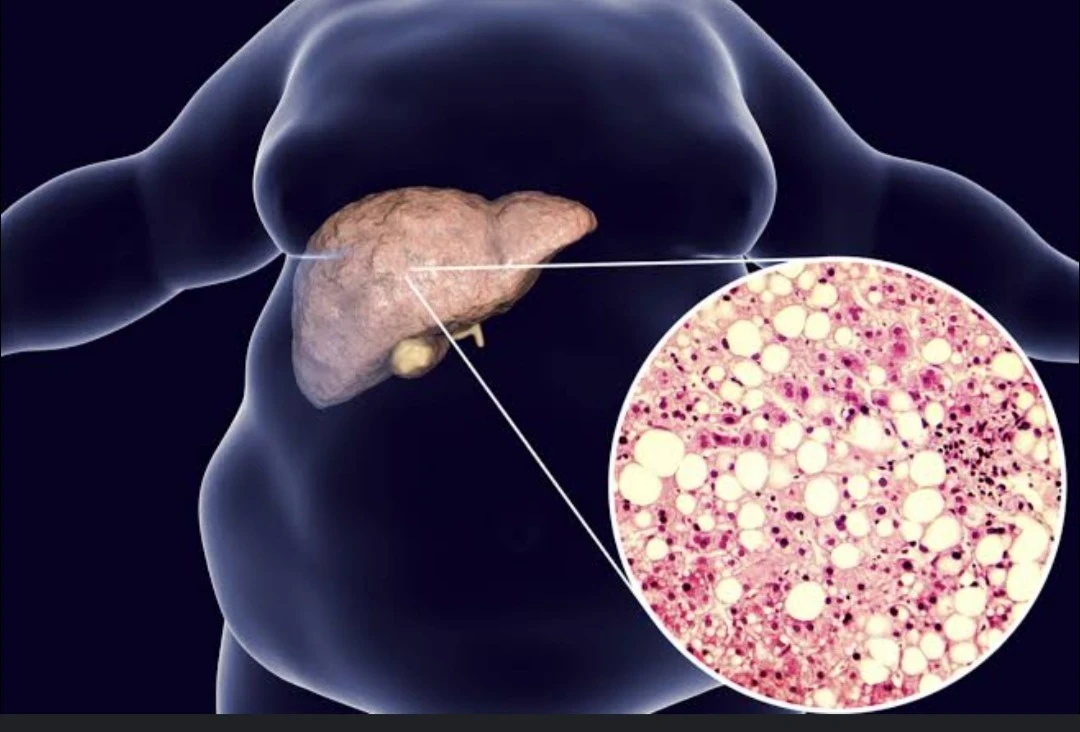
The liver is one of the hardest-working organs in the human body. It filters toxins, processes nutrients, stores vitamins, and helps regulate metabolism. But when fat starts to build up inside liver cells, it can disrupt these processes and eventually damage the liver. This condition is known as fatty liver or hepatic steatosis.
But is fatty liver just a symptom—or is it an actual disease? The answer is nuanced.
Fatty Liver as a Symptom
In some cases, a fatty liver is simply a sign—or symptom—that the body is struggling with another underlying condition. For example, people with obesity, insulin resistance, or uncontrolled type 2 diabetes often develop fatty liver as a secondary problem. In this context, fatty liver is more of a warning sign that the body’s metabolism is out of balance.
Fatty Liver as a Disease
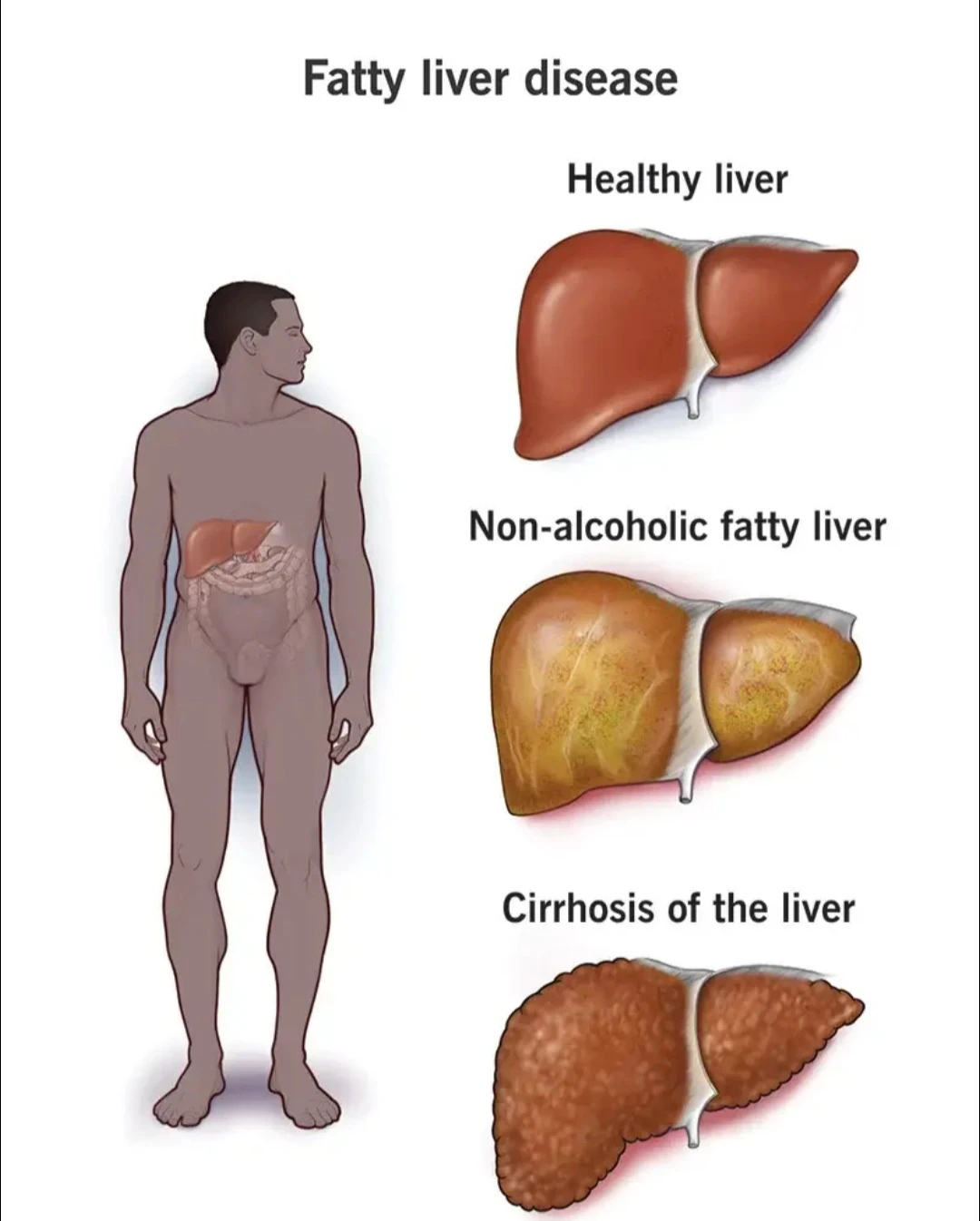
On the other hand, fatty liver can also progress into a full disease with serious consequences. When fat accumulation becomes severe, it can cause inflammation in the liver, a condition known as steatohepatitis. Over time, this inflammation can lead to fibrosis (scarring of the liver), cirrhosis (severe scarring that impairs liver function), and even liver cancer.
This is why experts often classify fatty liver into two categories:
1. Non-Alcoholic Fatty Liver Disease (NAFLD) – when fat accumulates in the liver due to metabolic issues, not alcohol.
2. Alcoholic Fatty Liver Disease (AFLD) – when heavy alcohol consumption is the primary driver.
Both forms start with fat buildup, but the progression and risks can be very different.
So in short: fatty liver is both a symptom and a disease. At first, it may just signal that something is wrong with your lifestyle or metabolism. But if ignored, it becomes a progressive disease that threatens overall health.
---
Why Are More People Living With Fatty Liver Than Ever Before?
You may be wondering: if fatty liver has been around for centuries, why are so many more people struggling with it today? The answer lies in the intersection of modern lifestyle, diet, and environment.
1. The Global Obesity Epidemic
One of the biggest drivers of fatty liver is obesity. As waistlines have expanded worldwide, fatty liver has followed closely behind. In fact, studies suggest that up to 70% of obese individuals also have fatty liver disease.
The problem isn’t just about weight—it’s about how the body stores and processes fat. When the body has more fat than it can handle, especially around the abdomen, it starts depositing fat in organs like the liver.
2. Sedentary Lifestyles
Modern technology has made life more convenient—but also less active. Many people spend hours sitting at desks, working on computers, or scrolling through their phones. Lack of physical activity means fewer calories burned and more fat stored, which contributes directly to fatty liver development.
3. Unhealthy Diets (The “Western Diet”)
Fast food, sugary drinks, refined carbs, and processed snacks dominate modern diets. These foods are high in sugar and unhealthy fats, and they spike insulin levels. Over time, this leads to insulin resistance, a major risk factor for fatty liver.
Particularly harmful is fructose, a sugar found in sweetened beverages and processed foods. Unlike glucose, fructose is primarily metabolized in the liver, where it easily turns into fat. This explains why frequent soda drinkers are at high risk for developing fatty liver.
4. Rising Rates of Type 2 Diabetes and Metabolic Syndrome
Type 2 diabetes and metabolic syndrome are both closely linked to fatty liver. People with insulin resistance—the body’s inability to use insulin effectively—often store excess fat in the liver. As rates of diabetes continue to climb globally, fatty liver cases climb alongside them.
5. Alcohol Consumption Patterns
Even though non-alcoholic fatty liver disease is now more common than alcoholic fatty liver, rising alcohol consumption in some regions also plays a role. Regular heavy drinking stresses the liver and accelerates fat buildup.
6. Environmental and Genetic Factors
Some people are genetically predisposed to store fat in their liver more easily than others. Additionally, exposure to environmental toxins, pollution, and even certain medications can increase the risk.
7. Better Awareness and Diagnosis
Finally, part of the reason more people are being diagnosed today is simply better detection. Decades ago, many people with fatty liver went undiagnosed because imaging technology (like ultrasounds and MRIs) wasn’t as widely used. Today, doctors are screening more aggressively, leading to higher reported cases.
---
A Modern Epidemic
Put simply: the rise of fatty liver is a modern epidemic, driven by the way we eat, live, and manage our health. It has become one of the most common liver conditions in the world, affecting an estimated 1 in 4 adults globally. In children and teenagers, rates are also climbing due to rising obesity.
This makes fatty liver not just a personal health issue, but a public health challenge that demands more awareness, prevention, and treatment strategies.
Causes of Fatty Liver
Fatty liver rarely develops without reason. In most cases, it reflects a combination of lifestyle, environment, and genetic influences that gradually overwhelm the liver’s ability to process fats. Understanding these causes makes it easier to prevent and treat the condition.
Obesity and Excess Weight
Excess body fat, especially abdominal fat that surrounds internal organs, is one of the strongest predictors of fatty liver. When fat storage in other tissues reaches capacity, the body begins to deposit fat in the liver. This process is common in people who are overweight, but it can also affect those with normal weight who carry excess visceral fat.
Insulin Resistance and Type 2 Diabetes
Fatty liver and diabetes are closely connected. In insulin resistance, cells do not respond effectively to insulin, so the pancreas produces more of it. Elevated insulin levels encourage fat storage in the liver. Around two-thirds of people with type 2 diabetes are estimated to have fatty liver, and the condition often appears before diabetes is officially diagnosed.
Unhealthy Diets
Modern diets high in sugar, refined carbohydrates, and processed fats put enormous pressure on the liver. Sugary beverages and foods high in fructose are especially harmful because fructose is metabolized directly in the liver, where it is easily turned into fat. Diets dominated by fast food, white bread, pastries, and processed snacks promote weight gain, inflammation, and fat buildup in the liver.
Alcohol Consumption
Alcohol remains a direct and powerful cause of fatty liver. Excessive drinking changes how the liver processes fats and proteins, leading to fat accumulation. Even moderate drinking can worsen pre-existing fatty liver caused by other factors. Continued alcohol intake raises the risk of alcoholic hepatitis, fibrosis, cirrhosis, and ultimately liver failure.
Medications and Toxins
Certain medications can contribute to fatty liver by interfering with fat metabolism. Corticosteroids, chemotherapy drugs, antiretroviral therapy, and some heart medications are examples. The condition usually improves when the medication is adjusted or discontinued under medical supervision.
Rapid Weight Loss and Malnutrition
While obesity is a major cause, the opposite extreme—losing weight too quickly—can also overload the liver with fatty acids. Similarly, protein deficiency and chronic malnutrition impair the liver’s ability to process fat.
Genetic Predisposition
Some people are genetically more likely to develop fatty liver, even at a healthy weight. Specific populations, such as those of Hispanic or South Asian descent, have higher prevalence rates, suggesting that inherited traits play a significant role.
Hormonal Disorders
Conditions such as polycystic ovary syndrome (PCOS), hypothyroidism, and Cushing’s syndrome are associated with fatty liver because of the hormonal imbalances they create. These imbalances disrupt metabolism and promote fat accumulation.
Gut Microbiome and Inflammation
Emerging research shows that an unhealthy gut microbiome may produce compounds that increase inflammation and fat storage in the liver. This connection highlights the importance of gut health in overall liver health.
---
Types of Fatty Liver
Fatty liver exists on a spectrum that ranges from mild to severe. Identifying the type and stage is essential for understanding the risks and guiding treatment.
Alcoholic Fatty Liver Disease (AFLD)
This type is caused by excessive alcohol intake. Alcohol disrupts fat metabolism, leading to accumulation in the liver. If drinking continues, AFLD can progress to alcoholic hepatitis, fibrosis, cirrhosis, and even cancer. The most effective treatment is complete abstinence from alcohol.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD develops in people who drink little or no alcohol. Instead, it is driven by obesity, diabetes, poor diet, and metabolic syndrome. It is now the most common liver condition worldwide.
NAFLD has several stages:
1. Simple steatosis – fat in the liver with little or no inflammation.
2. Non-Alcoholic Steatohepatitis (NASH) – fat plus inflammation and liver cell damage.
3. Fibrosis – scarring begins to replace healthy tissue.
4. Cirrhosis – severe scarring that limits liver function.
5. Liver cancer – in advanced cases, cirrhosis can progress to hepatocellular carcinoma.
Acute Fatty Liver of Pregnancy
This rare but dangerous condition occurs in the third trimester of pregnancy. It requires urgent medical attention, as it can cause liver failure if untreated.
Drug-Induced Fatty Liver
Some medications can directly cause fat buildup in the liver. This type is usually reversible once the drug is discontinued.
Pediatric Fatty Liver Disease
Fatty liver is no longer an adult-only condition. Rising rates of childhood obesity have led to increasing cases of NAFLD in children and teens. Worryingly, it can progress to NASH and fibrosis even at a young age.
Symptoms of Fatty Liver
One of the most challenging aspects of fatty liver disease is that it is often called a “silent condition.” In its early stages, most people experience little to no noticeable symptoms. The liver has a remarkable ability to keep functioning even when damaged, which means fatty liver can go unnoticed for years.
However, as fat accumulation and inflammation progress, symptoms may begin to appear.
Common Early Symptoms
Fatigue: Feeling unusually tired or lacking energy is one of the most reported complaints.
Discomfort in the upper right abdomen: A dull ache or pressure beneath the ribs where the liver sits.
Mild digestive issues: Such as bloating, nausea, or loss of appetite.
Symptoms in Advanced Stages
When fatty liver progresses to more serious conditions like non-alcoholic steatohepatitis (NASH), fibrosis, or cirrhosis, symptoms become more noticeable:
- Unexplained weight loss
- Persistent abdominal pain
- Weakness or muscle loss
- Swelling in the legs (edema)
- Enlarged liver or spleen
- Jaundice (yellowing of the skin and eyes)
- Easy bruising or bleeding
- Confusion or difficulty concentrating (in severe cases where toxins build up in the blood)
The Problem of Silent Progression
Because fatty liver often shows few warning signs, many people only discover it during routine blood tests or imaging for unrelated health issues. This silent progression makes regular checkups vital for anyone at risk—especially those who are overweight, diabetic, or heavy drinkers.
---
Diagnosis of Fatty Liver
Doctors use a combination of history, physical examination, imaging, and sometimes biopsy to confirm fatty liver.
Medical History and Risk Assessment
The first step is usually a detailed discussion of lifestyle, alcohol intake, diet, weight changes, and family history. Doctors also check for conditions linked to fatty liver such as diabetes, high cholesterol, or hypertension.
Blood Tests
While no blood test can directly confirm fatty liver, certain results may raise suspicion:
Elevated liver enzymes (ALT, AST, GGT)
High triglycerides and cholesterol
Elevated fasting glucose or HbA1c (a sign of insulin resistance or diabetes)
However, some people with fatty liver have normal enzyme levels, so blood work alone is not reliable.
Imaging Tests
Imaging is often used to visualize fat in the liver:
Ultrasound: The most common tool, showing a “bright” liver when fat is present.
CT scan and MRI: Provide more detail but are more costly.
FibroScan (Transient elastography): A specialized ultrasound that measures both fat content and liver stiffness, useful for detecting fibrosis.
Liver Biopsy
In uncertain or severe cases, a biopsy may be performed. A small tissue sample is taken and examined under a microscope to confirm fat content, inflammation, and scarring. While invasive, this remains the gold standard for distinguishing simple fatty liver from NASH.
---
Complications of Fatty Liver
Not everyone with fatty liver develops serious problems. In fact, many people with simple steatosis may never experience liver-related complications. But for others, especially those with NASH, the disease can progress and cause major health issues.
Steatohepatitis (NASH)
When fat accumulation is accompanied by inflammation and cell damage, the condition escalates to non-alcoholic steatohepatitis (NASH). NASH is far more dangerous than simple fatty liver because inflammation drives scarring and long-term damage.
Fibrosis
Ongoing inflammation leads to fibrosis, where scar tissue begins to replace healthy liver cells. Fibrosis restricts blood flow and liver function. At this stage, some damage may still be reversible with lifestyle changes.
Cirrhosis
If fibrosis becomes severe and widespread, cirrhosis develops. This stage is marked by extensive scarring that permanently reshapes the liver, severely limiting its function. Cirrhosis can cause complications such as:
Portal hypertension (increased pressure in liver blood vessels)
Varices (swollen veins in the esophagus or stomach, which can rupture and bleed)
Fluid buildup in the abdomen (ascites)
Liver failure
Liver Cancer
Cirrhosis greatly increases the risk of hepatocellular carcinoma, a primary liver cancer. Patients with long-standing NASH or alcoholic cirrhosis are at particularly high risk.
Extrahepatic Complications
Fatty liver is not only about the liver. It is closely tied to whole-body metabolic health, increasing the risk of:
Cardiovascular disease (heart attacks, strokes)
Type 2 diabetes progression
Chronic kidney disease
In fact, many people with fatty liver do not die from liver failure but from heart-related complications.
---
The Role of Clinical Nutrition in Fatty Liver Management
While medications for fatty liver are still being researched, nutrition and lifestyle changes remain the cornerstone of treatment. Clinical nutrition focuses on using dietary strategies tailored to each patient’s needs, with the goal of reducing liver fat, controlling weight, and preventing progression.
Weight Management
Losing even 5–10% of body weight can significantly reduce liver fat and inflammation.
Gradual weight loss is best—around 0.5–1 kg per week.
Rapid crash diets should be avoided because they can worsen liver problems.
Macronutrient Balance
Carbohydrates: Focus on complex carbs like whole grains, legumes, and vegetables. Limit refined carbs and added sugars.
Proteins: Lean protein sources such as fish, poultry, beans, and tofu help support liver repair and satiety.
Fats: Replace saturated and trans fats with healthy fats from olive oil, nuts, seeds, and fatty fish (rich in omega-3).
Foods That Support Liver Health
Vegetables and fruits: High in antioxidants and fiber. Leafy greens, berries, and cruciferous vegetables (broccoli, cauliflower) are especially beneficial.
Coffee: Research suggests moderate coffee consumption may lower the risk of fibrosis.
Green tea: Contains catechins, compounds linked to fat reduction and improved liver health.
Omega-3 fatty acids: Found in salmon, mackerel, flaxseeds, and walnuts, which reduce inflammation and triglycerides.
Foods to Limit or Avoid
Sugary drinks and fruit juices
Processed snacks and fast food
Alcohol
White bread, pastries, and pasta made from refined flour
High-fat fried foods
Clinical Nutrition Plans
Dietitians may create personalized meal plans that:
- Reduce calorie intake in a sustainable way
- Emphasize liver-friendly foods
- Address co-existing conditions like diabetes or high cholesterol
- Provide education on reading food labels, portion sizes, and meal timing
Beyond Diet: Lifestyle Factors
Physical activity: At least 150 minutes of moderate-intensity exercise per week helps reduce liver fat even without major weight loss.
Sleep: Poor sleep and sleep apnea worsen insulin resistance and fatty liver.
Stress management: Chronic stress can affect hormones and eating behaviors, indirectly worsening liver health.
---
Why Nutrition Is Central to Treatment
Unlike some chronic conditions that require heavy reliance on medications, fatty liver can be slowed, halted, or even reversed through nutrition and lifestyle adjustments. For many patients, diet is not just supportive care—it is the most powerful therapy available today.
Conclusion: Taking Charge of Fatty Liver Health
Fatty liver disease is no longer a rare condition—it’s become one of the most common liver concerns worldwide. The rise in cases is closely linked to modern lifestyle patterns: diets rich in refined sugars and unhealthy fats, less physical activity, increasing obesity rates, and higher stress levels. While many people first learn they have fatty liver through routine tests and may feel anxious about the diagnosis, the encouraging truth is that fatty liver is largely reversible when addressed early.
Understanding the difference between a symptom and a disease helps us see why proactive management is crucial. For some, fatty liver may reflect another underlying condition such as diabetes, insulin resistance, or alcohol misuse. For others, it is the starting point of a progressive liver disorder. Either way, catching it early prevents complications like cirrhosis or liver cancer down the line.
Diagnosis today is easier than ever, thanks to imaging tools, lab tests, and risk assessments that help healthcare providers identify the severity and type of fatty liver disease. Once diagnosed, treatment focuses on lifestyle interventions. Medications are being studied, but nutrition and daily habits remain the foundation of care.
This is where clinical nutrition plays its vital role. A carefully planned diet—rich in whole foods, vegetables, fruits, lean proteins, and healthy fats—supports liver healing, reduces fat deposits, and improves metabolic health. Equally important is avoiding processed foods, sugary drinks, alcohol, and excess calories. When combined with regular exercise, stress management, and consistent medical follow-ups, nutrition becomes a powerful therapeutic tool, not just a supportive measure.
In essence, fatty liver does not have to define your health journey. With awareness, the right lifestyle adjustments, and medical guidance, you can protect your liver, restore its vitality, and prevent long-term complications. Think of fatty liver not as the end of health, but as a wake-up call—an opportunity to take charge of your wellbeing, make better choices, and give your liver the care it deserves.